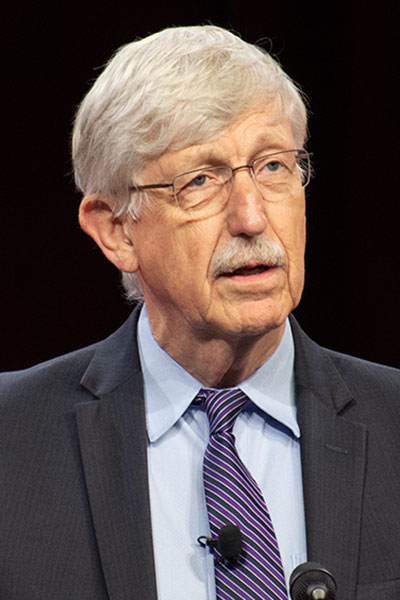
Omics data enables investigators to study the human genome more precisely than ever before and could lead to significant advances in research and therapies for diabetes, according to Francis S. Collins, MD, PhD. In his opening keynote lecture at the 83rd Scientific Sessions, “The Omics Revolution Provides New Insights for Diabetes,” Dr. Collins highlighted how omics data is already impacting the understanding of the disease at a molecular level.
The session can be viewed on-demand by registered meeting participants at ADA2023.org. If you haven’t registered for the 83rd Scientific Sessions, register today to access the valuable meeting content through August 28.
Dr. Collins became the second director of the National Center for Human Genome Research at the National Institutes of Health (NIH) in April 1993. He led the Human Genome Project, which generated the first sequence of the human genome blueprint, accelerating the study of human biology and opening new opportunities in precision medicine. He compared the significance of this project to the moon landing and the splitting of the atom.
“One of the things that we focused on, of course, was the opportunity to use information about human variation to begin to take apart the complexities of common diseases like diabetes,” he explained.
One result of this research was the development of genome-wide association studies (GWAS), which use information about common variations in the genome to identify statistically significant differences between people with a given disease and those without. Such data can be used to identify differences in the expression of type 1 diabetes and type 2 diabetes.
“We need to break down type 2 diabetes and type 1 diabetes into what you might call endotypes or different kinds of subsets. Now, they’re going to have different natural histories, perhaps, a different response to prevention and treatment modalities, and it’s time to get beyond the lumping and do some splitting,” Dr. Collins said.
One aspect of emerging omics research that Dr. Collins characterized as a “game-changer” is the ability to study single cells versus bulk tissue. Individual cells are different, and if researchers are averaging the data in bulk tissues, it could lead to the omission of significant insights on a deeper level, he said.
Dr. Collins also said the use of stem cells as a window in beta-cell technology was a major development over the past 15 years. He cited an impressive application of these methods by the New York Stem Cell Foundation, which used an automated platform to differentiate patient-induced pluripotent stem cells (iPSCs) to mature stem cell-derived pancreatic islets (SC-islets). This means researchers can study a patient’s pancreatic islets without having to perform a risky and invasive biopsy or wait until after the patient has died.
Since most of this research is still in a relatively early stage, Dr. Collins highlighted emerging clinical applications for specialists who treat patients with diabetes. For rare forms of the disease, he encouraged participation in the Rare and Atypical Diabetes Network (RADIANT). Studying unique phenotypes that include diabetes as part of their presentation might lead to new genetic insights that were previously undetectable.
Pharmacogenomics, the study of how genes affect a person’s response to drugs, is another area that will be significantly impacted by genetic research. The goal of this field is to develop medications and doses tailored to an individual’s genetic makeup.
Another emerging clinical application Dr. Collins cited was polygenic risk scores, which calculate an individual’s total number of genetic variants to assess the risk of a particular disease.
Dr. Collins is currently focused on eliminating hepatitis C, a disease that affects over 2 million people in the United States. It is curable, but due to factors such as lack of awareness, high costs of treatment, and insurance restrictions, progress has been limited, he noted. He’s now working directly with the Biden administration on a five-year plan to reach, test, and cure 2 million patients with hepatitis C. His three-point plan includes developing a point-of-care test, making drug access essentially free for those who can’t afford it, and providing health care delivery resources to reach marginalized groups.
He shared that research has shown one of the benefits of curing hepatitis C is a significantly reduced risk of diabetes. A study he cited showed that patients were at a 74% lower risk for diabetes after treatment for hepatitis C.
Dr. Collins concluded his presentation with a message of optimism and encouragement: “The science that all of you are doing and the way in which the clinical folks are bringing that to bear are enabling a revolution in our ability to understand, prevent, and treat this disease,” he said.